Collaborative Approaches to Global Mental Health Solutions
Overview
- Students and grandparents are stepping up to lead mental health initiatives.
- Innovative programs in Africa offer scalable models for the rest of the world.
- Community health workers are essential for improving mental health access.
A Community-Based Model in Kenya
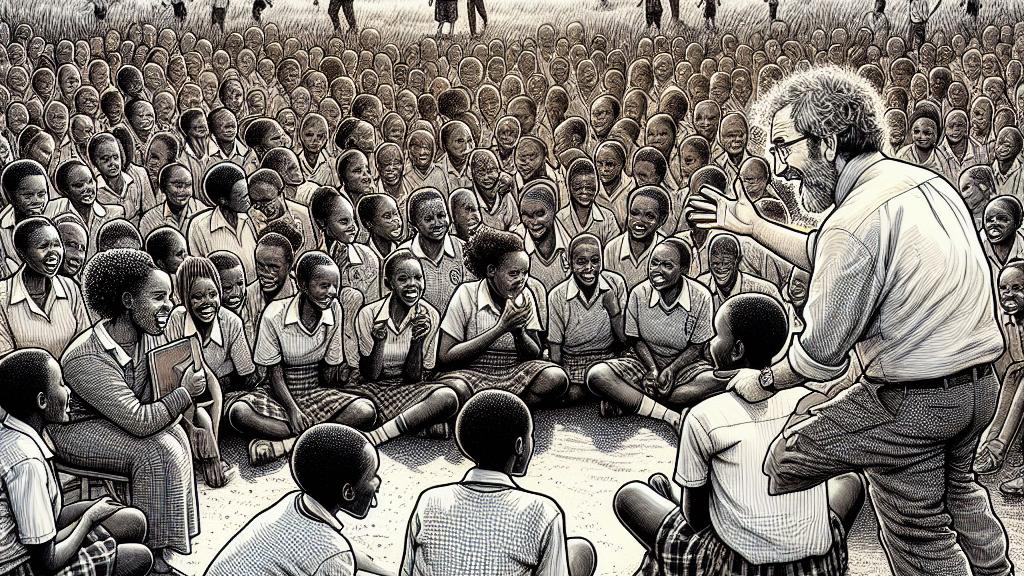
Imagine descending onto a sunlit field at Archbishop Okoth Ojolla Girls’ High School in Kisumu, Kenya—here, 900 spirited students gather with the promise of healing. Local graduates, trained by the Shamiri Institute, engage their peers in meaningful therapy sessions, fostering an atmosphere where vulnerability is met with understanding. This innovative approach arises from the staggering reality of fewer than 2 mental health professionals per 100,000 people in the region. Whitney Ndemo, a supervising psychologist, speaks passionately of one student, a boy who, after experiencing immense trauma, found solace among his peers in these sessions. Such stories underscore the profound impact of community-driven support, proving that when students rally together, they can change lives.
Global Implications of Lay Provider Models
The transformative strategies being piloted in Kenya sound a clarion call for nations worldwide. Researchers are discovering that lay providers, including trained youth and compassionate elders, can deliver effective mental health care, sometimes even achieving better results than traditional professionals. Embracing these approaches necessitates a shift in perspective: mental health care can, and should, take place within communities rather than just in isolated clinics. Countries eager to alleviate mental health crises are observing this inspiring model. However, let’s not ignore the inherent challenges, such as managing burnout among these lay providers and ensuring quality control. Yet, the potential benefits of community integration illuminate a path towards alleviating the mental health burden that countless individuals face.
Empowering Communities through Health Workers
Let’s take a moment to shine a light on the unsung champions—Community Health Workers (CHWs)—who play a pivotal role in bridging gaps in mental health care. These dedicated individuals metaphorically hold the hands of those who feel lost, guiding them through the often confusing healthcare pathways. By providing culturally attuned support, CHWs help dismantle barriers that continue to prevent many from seeking help. For instance, in rural regions, they tackle chronic conditions while simultaneously addressing mental health needs, ensuring that patients are equipped with the tools they need to thrive. In bustling urban areas, they frequently organize outreach initiatives that focus on destigmatizing mental health discussions, converting fear into understanding. The tangible impact they achieve emphasizes a crucial lesson: when communities are involved, and voices are united, real progress in mental health accessibility becomes a tangible reality.

Loading...