Balancing Act: Pseudomonas Aeruginosa's Strategies Against Antibiotics
Overview
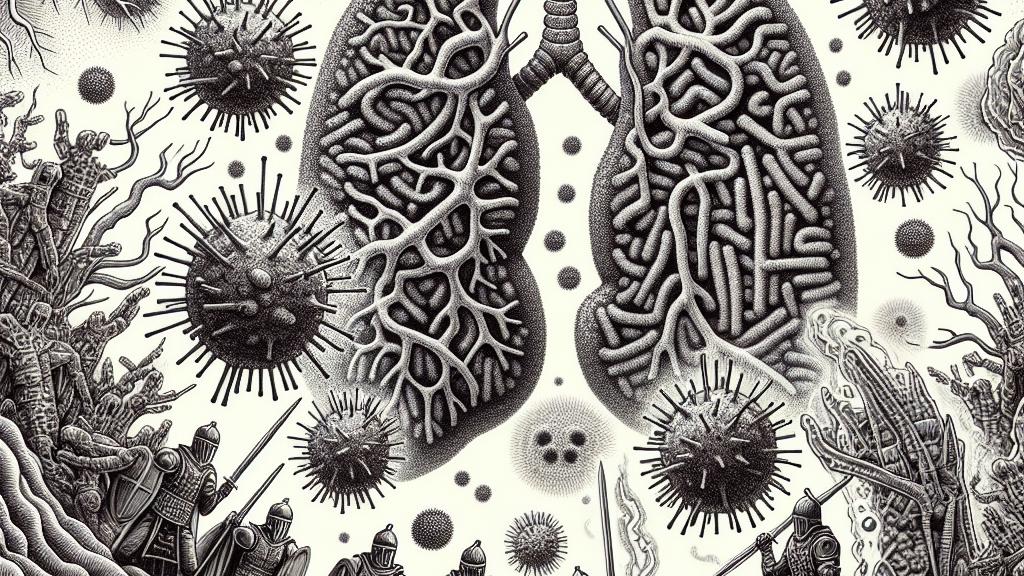
- Pseudomonas aeruginosa faces a critical dilemma: colonizing lung tissue while evading the effects of antibiotics.
- Biofilms provide robust protection but simultaneously hinder the bacterium's movement and nutrient acquisition.
- Emerging research reveals this delicate balance, paving the way for innovative treatment solutions to combat antibiotic resistance.
Surviving in Hostile Environments
Pseudomonas aeruginosa is a notorious pathogen, particularly feared in hospital settings, where it can thrive in moist areas such as sinks and catheters. This Gram-negative bacterium is notorious for causing severe, often life-threatening infections, especially in vulnerable patients with conditions like cystic fibrosis. Imagine this tiny organism trying to stake its claim in the lungs, a hostile environment filled with immune defenses and antibiotics. It faces a daunting question: Should it prioritize spreading throughout the lung tissue or fortifying its defenses against therapeutic attacks? This internal conflict highlights the critical balancing act P. aeruginosa must perform, a dance dictated by survival instincts and environmental pressures.
The Complex Role of Biofilms
Biofilms are among the most brilliant survival strategies employed by Pseudomonas aeruginosa. These dense clusters of bacteria not only shield the microbes from immune responses but also provide a formidable barrier against antibiotics. However, these protective structures come at a price. Recent studies from the Ecole Polytechnique Federale de Lausanne (EPFL) have shown that the formation of biofilms imposes a significant 'metabolic burden'—meaning the resources required to create and maintain these clusters slow down the bacteria's ability to gather nutrients and move effectively. For example, while biofilms can protect P. aeruginosa during antibiotic treatment, they limit its adaptability in less hospitable environments, creating a complex interplay between protection and vulnerability.
Exploring New Frontiers in Treatment
The insights gained from understanding how Pseudomonas aeruginosa balances its survival strategies open exciting avenues for medical advances. Imagine if clinicians could disrupt biofilm formation or specifically target cells in their planktonic state to enhance the efficacy of existing antibiotics. Such strategies could lead to revolutionary treatments that dramatically improve patient outcomes. For instance, combining antibiotics with enzymes designed to break down biofilm structures may render these infections much easier to treat. Furthermore, by investigating the metabolic pathways utilized by P. aeruginosa in the lung environment, researchers can design novel therapies that prevent the bacterium from thriving during critical stages of infection. This ongoing research underscores the importance of innovative strategies in the fight against antibiotic resistance, ultimately contributing to a healthier future by protecting patients from the threats posed by resistant bacteria.

Loading...