Revolutionary Antibody: The Game Changer in PD-L1 Blockade!
Overview
- Breakthroughs in anti-TIGIT antibodies enhance PD-L1 blockade efficacy.
- Myeloid cells and Tregs play pivotal roles in immunotherapy response.
- Clinical trials showcase promising results for advanced solid tumor treatments.
Innovative Advances in Cancer Immunotherapy
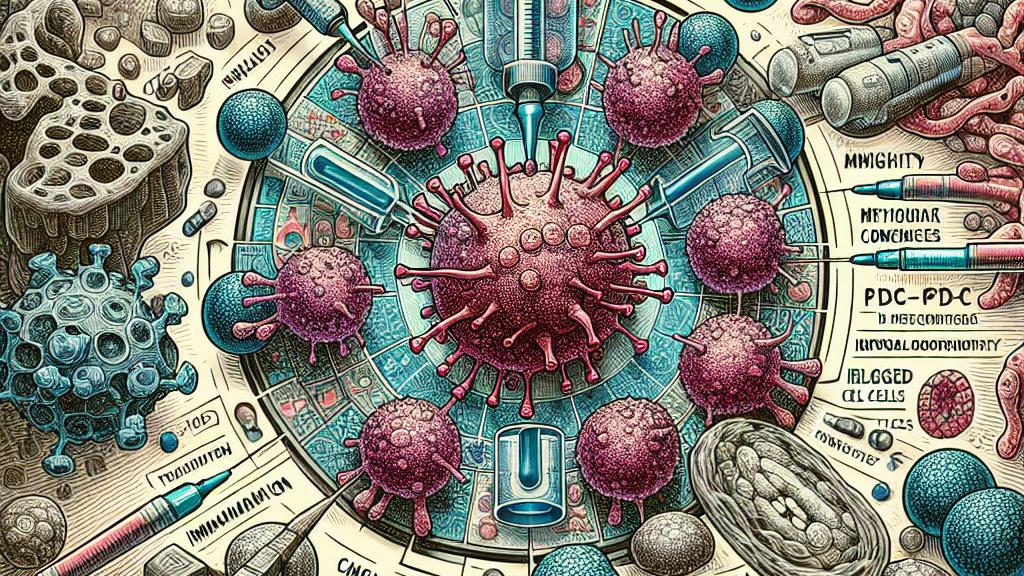
Recent studies from the USA have unveiled exciting advancements in treating non-small-cell lung cancer (NSCLC) through the use of anti-TIGIT antibodies. This research highlights how these antibodies significantly improve the effectiveness of PD-L1 blockade, a common therapeutic strategy. The combination of anti-TIGIT antibodies with existing treatments could revolutionize how we approach the challenges in immunotherapy. Understanding the key roles that myeloid cells and regulatory T cells (Tregs) play are essential in enhancing the therapeutic response, which presents an opportunity to develop more tailored treatment regimens for patients with advanced solid tumors.
Clinical Trials: A Testbed of Promising Results
In a landmark first-in-human phase 1 trial, the anti-TIGIT antibody vibostolimab was evaluated alone and in conjunction with pembrolizumab for patients battling advanced solid tumors. Results from the trial indicate that patients receiving the combination therapy exhibited a noteworthy objective response rate, particularly among those who were previously untreated with PD-1/PD-L1 therapies. The high tolerance for this regimen, accompanied by a manageable safety profile, suggests that combining therapies could provide a robust and effective strategy to tackle tumor resistance, paving the way for better therapeutic outcomes and survival rates in patients.
Future Directions: Optimizing Immunotherapy Approaches
As the landscape of cancer treatment continually evolves, the focus on the mechanisms of immune checkpoint inhibitors like anti-TIGIT antibodies becomes increasingly important. Researchers are now actively investigating the roles of myeloid-derived suppressor cells (MDSCs) and regulatory T cells (Tregs) in shaping the outcomes of therapies that target PD-1/PD-L1. These insights could inform innovative therapeutic strategies that not only enhance the efficacy of existing treatments but also reduce adverse effects. Ultimately, combining new technologies and approaches with traditional immunotherapy strategies holds the potential to redefine the standards of cancer care, offering hope for improved patient outcomes.

Loading...